Abstract
Background Detection of anaemia is critical for clinical medicine and public health in high and low income settings, but anaemia definitions are uncertain, causing discordance across different laboratories and guidelines. Current WHO anaemia definitions, set in 1968 using limited data, reflect the 5th centile of the haemoglobin distribution in apparently healthy populations. WHO is now reviewing these definitions. Haemoglobin concentration is sensitive to iron and other nutrient deficiencies, inflammation, renal impairment, and genetic conditions, and thus conservative criteria to obtain a healthy reference population is crucial in estimating the 5th centile. To support WHO definitions, this study estimated the 5th centile for haemoglobin in healthy reference populations derived from a secondary analysis of large cohorts.
Methods We identified data sources from which sufficient clinical and laboratory data were available to identify an apparently healthy reference sample. These comprised the National Health and Nutrition Examination Survey (NHANES, USA, 8 survey years); Health Survey for England (HSE, England, 4 survey years); the Australian Health Survey (AHS), comprising 2 separate surveys: National Health Survey (NHS, Australia) and National Nutrition and Physical Activity Survey (NNPAS, Australia); TARGetKids! (prospective longitudinal cohort of children, Canada); BRISC (trial of oral iron in infants, Bangladesh); Generation R (prospective cohort of pregnant women, Netherlands). Markers or iron status and inflammation were available in all surveys, with exclusions for ferritin<15ug/L (or <12ug/L in children <5 years), or C-Reactive Protein (CRP) >5mg/L. Where possible, exclusions were applied based on renal function, folate, and active B12. Clinical data from all surveys (except Generation R) excluded individuals with pre-existing health conditions, use of medication (other than contraception), recent illness or hospital admission. In the pregnant Generation R group, those with pregnancy complications were excluded. In all groups, current smokers and those who consumed excess alcohol were excluded. Adults with BMI <18.5 or >30kg/m2 were excluded; children were excluded if growth z-scores were <-2 or >+2. In children <24months, those with birth complications or prematurity were excluded.
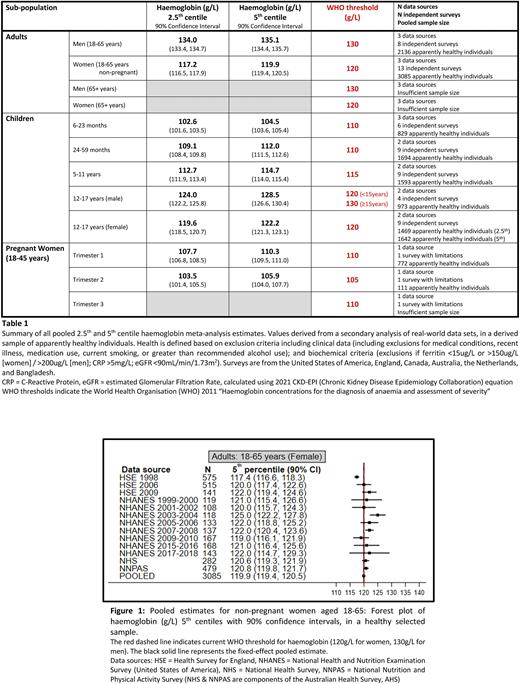
Thresholds were defined in adult men (18-65 years), adult non-pregnant women (18-65 years), pregnant women (18-45 years, by trimester), and children (6-23 months, 24-59 months, 5-11 years, 12-17 years). Discrete 2.5th and 5th centiles were estimated along with two-sided 90% confidence intervals for each data set and estimates were combined across all data sources using a fixed-effect meta-analysis approach.
Results In non pregnant adult men and women (total n=57,896 individuals), exclusions resulted in an apparently healthy group of 15-20% of each survey (less where survey years were missing required biochemistry). A broad range of self-reported ethnicities/ancestries were represented. For example in healthy adults: NHANES 17-33% of participants identified as White; HSE >90% identified as White; AHS 50-60% reported European ancestry.
5th centiles of the distribution of haemoglobin values in the derived reference samples were obtained (see Figure 1 for example in non-pregnant women). Pooled estimates for each sample are shown in Table 1. The results generally align with current WHO thresholds, other than adult men, where a 5th centile of 135.1g/L (90% CI 134.4-135.7) is above the WHO threshold of 130g/L, and in children 6-23 months where the 5th centile of 104.5g/L (90% CI 103.6-105.4) is lower than the current value of 110g/L. Our data support the current threshold in non-pregnant adult women of 120g/L. Sensitivity analyses suggest persons of Black race or ethnicity may have 5th centiles lower than values of White persons (predominantly within the US surveys), but presence of haemoglobinopathy as well as other contributing factors cannot be excluded.
Conclusion In this analysis using stringent criteria to define healthy reference group at low risk of iron/ other nutrient deficiency, or inflammation, we have estimated statistical thresholds to define anaemia across the lifecycle. These data contribute to WHO guideline development, and provide a platform for harmonisation of thresholds across different laboratories and clinical guidelines.
Disclosures
Pasricha:Vifor Pharma: Consultancy; Keros Therapeutics: Consultancy.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal